Social, Psychological, and Diagnostic Aspects of Depression in Men
Four times more men die by suicide than women, and yet half as many men are diagnosed with depression as are women (1). In researching this topic, I was encouraged by the shift our society is making towards understanding depression in men and the factors that push them to such lengths. However, there is clearly still a long way to go. A book I skimmed early on in my search, aptly titled Men and Depression, by Sam Cochrin and Frederic Rabinowitz, mentions in the introduction that “A book that examines distress and depression in men may be seen by some as politically provocative.” In 2000, when that book was published, many researchers and clinicians were working to move public perception of mental disorders in men inch by inch. They recognized that the disparity between the number of men diagnosed with depression and the number of men who kill themselves indicates a hidden population of men who battle their depression in secret. 21 years later, the number of articles under a “depression in men” search in Google Scholar numbers over 3.5 million.
As a woman who suffers from depression, I feel relatively safe in disclosing my diagnosis. People are generally sympathetic and understanding when I discuss my symptoms. But how do men feel about the way their depression is received? A man I know has been dealing with depression for a long time, so I asked him exactly that question. Thankfully, he told me that his social circles have been largely supportive, which I think is an encouraging sign for our culture’s direction. But what factors make the rates of suicide between men and women so different? If we’ve come from “politically provocative” to millions of research articles in two decades, why are many men still suffering in silence? I want to dig into this issue to understand the historical trends, what sometimes makes depression in men different, and what we can do to keep the conversation going.
Historical Epidemiology of Suicide
In a really deep dive, we could go way back to Hippocrates and Galen to explore the perceived gender divide on mental disorders, which would be interesting. But in this context, we’ll stick to the 20th and 21st centuries. Let’s take a look at this set of data from the CDC’s Data Finder (12). It’s compiled mostly by decade between 1950 and 2015. This graph of the data, which I made with my rusty skills in Excel, illustrates the suicide trends by rate among men in various age groups.
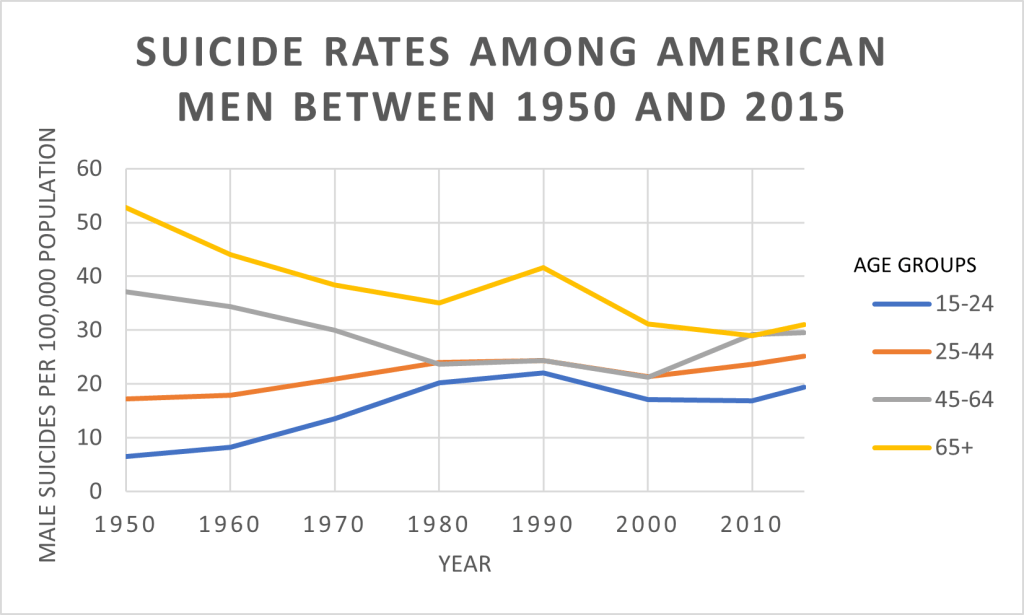
Although the rate of suicide among all ages has remained relatively stable, trends within age groups are concerning. Suicides among 15-24 year-olds have increased dramatically, as have those among 25-44 year-olds. Despite a somewhat steady decline in the suicide rate of men aged 65 and older, they remain the group with the highest rate. By 2019, the rate of suicide in men had increased from 21.1 deaths per 100,000 to 23 deaths per 100,000 (13). For every 100,000 men, 23 deaths doesn’t immediately sound shocking. But to illustrate the numbers in a different way, consider that in 2019, a horrifying total of 37,256 men killed themselves in the U.S.
It introduces another layer of complexity to compare the data on men to the data on women. The suicide rate among women of all ages has increased since the 50’s more than it has among men, but it still sits markedly lower. In 2019, the overall suicide rate among women was 6.2 deaths per 100,000 people (13). Compared to 37,256 male suicides, the country saw 10,255 female suicides. Both of those numbers are unimaginable to me, but it’s worth investigating; why is the rate for men so much higher than it is for women?

Diagnostic Factors
The wildly higher rate of suicides among men than in women, combined with the average 2:1 ratio of depression diagnoses in women versus men, convincingly suggests that depression in men is going undiagnosed. An increasingly accepted hypothesis regarding this conclusion is that depression in men and women can be experienced in different ways (10). The current diagnostic tools don’t capture all of the symptoms of depression that men commonly face. The gender differences in symptomatology have led some to argue for the recognition of separate depression diagnoses for men and women. Magovcevic and Addis conceptualized the differences as constituting typical depression plus a subtype, masculine depression (6). Subsequent research shows that some men who don’t fully fit the diagnostic criteria on traditional depression questionnaires may be diagnosed when masculine depression symptoms are considered.
Masculine Depression Symptoms
“Masculine depression” (also called male depression and a variety of other terms), is characterized by more symptoms of anger, aggression, risk taking, and substance abuse than tend to occur in women. These symptoms are examples of “externalizing features.” They serve to express a person’s emotions in an outward, active way. “Internalizing features” of depression are identified by retreating into one’s self, such as by ruminating, engaging in negative self-talk, and isolating from others.
New Self-Report Scales
To investigate the efficacy of adjusted self-report scales at identifying depression in men, researchers created the Gender Inclusive Depression Scale (GIDS) using two other male depression scales validated with small cohorts. When symptoms of masculine depression – the externalizing features – are included in a traditional diagnostic survey, the rates of depression diagnoses among men and women are not significantly different (7). In other words, the gender differences disappear. Another scale, the Male Depression Risk Scale (8), measures emotion suppression, drug use, alcohol use, anger and aggression, somatic symptoms, and risk-taking. The sensitivity of the MDRS is similar to that of the PHQ-9 in recent suicide attempt identification (9).
Why is Depression in Men Sometimes Different?
To be clear, it’s a continuum; many men are diagnosed with depression using traditional questionnaires. But for the ones who aren’t, the answer is probably based in gender norms. Men who have depression and who identify with traditional ideals of masculinity are more likely to experience masculine depression symptoms (4). In a society that has traditionally viewed men who express sadness as “weak” or “feminine,” it makes sense that sometimes, depression in men is displayed as anger or in attempts to cope with it through substances. Sadly, it’s more socially acceptable for men to express anger than sadness, self-doubt, or anxiety.

Why is the Suicide Rate Among Men so Much Higher?
If newer diagnostic scales indicate that the rates of depression in men and women are actually more alike than previously thought, what is going on with the suicide rates? Why would men die by suicide four times more often than women? It’s hard to know how many suicides could have been prevented by mental health intervention, but it’s logical to think that men who aren’t seeking counseling or who are dismissed without a diagnosis would be more likely to turn to suicide as the answer. Additionally, we know that although men complete suicide more often than women, women attempt it more often (11). Men tend to use more lethal methods, and for some men, the act of suicide represents an affirmation of strength and independence (2). It is crucial that we improve identification and treatment of depression in men (5).
A Note on “Masculine” and “Feminine”
With all of this discussion about a “masculine” depression facet, I have a small fear that readers of this post will leave feeling as though their diagnosis of depression must have been of the feminine kind. It’s not. It’s just depression – men, women, nonbinary people – it doesn’t impose judgment on your identity, it simply is. Just as men may experience more anger and impulsivity as part of their depression, women may be more likely to suffer body image issues and self-harm behaviors. But it’s a bell curve; just because men are more likely than women to exhibit anger as a sign of depression doesn’t mean that women can’t as well. Statistically, neither gender is more closely associated than the other is with the typical symptoms (8). The only gendered difference exists in the subset of “masculine” symptoms. The core set of symptoms that are covered in typical scales like the PHQ-9 remain the main diagnostic components of what we know depression to be. Expanding the criteria by creating a subset of symptoms more associated with men is just a way of widening the net in order to keep people from falling through the cracks.
For more reading on how men can view depression, suicide, and masculinity, check out this article. The author provides evidence for a variety of views that men hold about how mental health and suicide relate to masculinity.
Identifying Depression in Men Going Forward
For a long time, our definition of depression was too narrow. The research on gender differences in depression, which I have only barely scratched the surface of, is vast and still growing. Although the standard depression questionnaires remain focused on internalizing features to the exclusion of the externalizing ones, authorities on the matter have acknowledged the issue in other ways. The American Psychiatric Association has a webpage from 2005 that describes the early research and what to watch out for in men who may have depression. They now have a number of web pages, magazine articles, fact sheets, and books about men and depression. Someday, I hope that standard depression questionnaires will include measures for symptoms that men exhibit, but until then, we can continue to reduce stigma and spread the word about how depression in men can manifest.

You can pass online resources on to the men you know. You can talk about it with your doctor. You can listen to your friends, fathers, brothers, and sons. Assure them that having feelings doesn’t make them less of a man, it just makes them human.
Resources
- National Suicide Prevention Lifeline: 1-800-273-TALK (1-800-273-8255)
- Advice on looking out for friends: beyondblue.org
- Potential symptoms and tips for self-care: texashealth.org
- Information, resources, and community: headsupguys.org
Citations
- “By the Numbers: Men and Depression,” December 2015. https://www.apa.org/monitor/2015/12/numbers.
- Canetto, Sylvia Sara, and Anne Cleary. “Men, Masculinities and Suicidal Behaviour.” Social Science & Medicine 74, no. 4 (February 2012): 461–65.
- Cochran, Sam, V, and Frederic Rabinowitz E. Men and Depression: Clinical and Empirical Perspectives. Academic Press, 2000.
- Genuchi, Matthew. “Anger and Hostility as Primary Externalizing Features of Depression in College Men.” Psychological Sciences Faculty Publications and Presentations, August 1, 2015. https://scholarworks.boisestate.edu/cgi/viewcontent.cgi?article=1223&context=psych_facpubs.
- Keohane, Aisling, and Noel Richardson. “Negotiating Gender Norms to Support Men in Psychological Distress.” American Journal of Men’s Health, October 11, 2017. https://pubmed.ncbi.nlm.nih.gov/29019282/.
- Magovcevic, Mariola, and Michael Addis. “The Masculine Depression Scale: Development and Psychometric Evaluation.” APA PsycNet, 2008. https://psycnet.apa.org/record/2008-09203-001.
- Martin, Lisa, A, Harold Neighbors W, and Derek Griffith M. “The Experience of Symptoms of Depression in Men vs Women: Analysis of the National Comorbidity Survey Replication.” JAMA Psychiatry, October 2013. https://jamanetwork.com/journals/jamapsychiatry/fullarticle/1733742.
- Rice, Simon, M, and Anne-Maria Moller-Leimkuhler. “Development and Preliminary Validation of the Male Depression Risk Scale: Furthering the Assessment of Depression in Men” 151, no. 3 (December 2013): 950–58.
- Rice, Simon, M, John Ogrodniczuk S, David Kealy, and Zac Seidler E. “Validity of the Male Depression Risk Scale in a Representative Canadian Sample: Sensitivity and Specificity in Identifying Men with Recent Suicide Attempt.” Journal of Mental Health, November 2017, 132–40.
- Rutz, Wolfgang, Jan Walinder, and Lars Von Knorring. “Prevention of Depression and Suicide by Education and Medication: Impact on Male Suicidality.” International Journal of Psychiatry in Clinical Practice, January 8, 1997. https://www.tandfonline.com/doi/abs/10.3109/13651509709069204.
- Schumacher, Helene. “Why More Men than Women Die by Suicide.” BBC Future (blog), March 17, 2019. https://www.bbc.com/future/article/20190313-why-more-men-kill-themselves-than-women.
- “Table 30. Death Rates for Suicide, by Sex, Race, Hispanic Origin, and Age: United States, Selected Years 1950-2015.” CDC, 2017. https://www.cdc.gov/nchs/data/hus/2017/030.pdf.
- “Underlying Cause of Death, 1999-2019 Request.” Data Table. CDC WONDER. Accessed January 17, 2021. https://wonder.cdc.gov/controller/datarequest/D76.